My Health, My Care, My Home - healthcare framework for adults living in care homes
Framework providing a series of recommendations that aims to transform the healthcare for people living in care homes.
Introduction
Providing high-quality, personalised care that is consistent, safe, and meaningful, is the top priority for our health and social care services in Scotland today. This framework aims to provide direction and vision that will maximise the health and wellbeing of people living in care homes. It aims to ensure that people living in care homes experience this wherever they are living in Scotland. Therefore, the framework, and its recommendations, are aligned to the Health and Social Care Standards and takes a human rights based approach. In order to fully implement this framework, it will be necessary to ensure that workforce and other resources are in place to address local needs and circumstances.
Scotland's population is now at its highest level and is also growing steadily older. This is true of both people living in care homes and the workforce that provides healthcare. It is undoubtedly positive that people are living longer, however, some are living with increasingly complex health and care needs which may necessitate residing within a care home.
The care home sector in Scotland provides care for adults and older people, individuals with learning and physical disabilities, neurological illness, mental health conditions and brain injury. Some care homes also provide intermediate care and respite services for people on a temporary basis. Across each of these groups the healthcare needs of those living in care homes is becoming more complex and requires more specialist interventions.
The latest Public Health Scotland Care Home Census for Adults in Scotland (published December 2021) reports that there are 33,000 people living in 1,069 care homes for adults in Scotland. Of these, 91% are living in a care home for older people, and 64% are living with dementia (either medically or non-medically diagnosed). The mean age at admission into a care home for older people is 82 years.
The 2021 census also reports there are 157 care homes for people with learning disabilities, 52 for people with mental health conditions, and 36 for people with physical and sensory impairment. The remaining 15 care homes for adults in Scotland included those for acquired brain injury, alcohol and drug misuse, and blood-borne virus.
The requirements of those living in care homes go beyond physical health, and include social, psychological and spiritual care needs.
"Importance of retaining community links, relationships, family and friendships. The importance of this in helping to maintain good health cannot be understated."
The COVID-19 pandemic has undoubtedly had a significant impact on people who live and work in care homes, and their friends and families. Older people, individuals with a weakened immune system, and those living with long term medical conditions were all more vulnerable to severe illness from the infection.
There have also been historical factors pre-pandemic which have challenged the care home sector. These issues are well documented in the Independent review of adult social care in Scotland report (2021). It is essential that we learn from these experiences and build on some of the excellent innovative practice, integrated working and relationship-building which have arisen in parts of the country during the course of the pandemic.
Care homes are where people live and call home. They should expect the same level of involvement, choice and support for their health and wellbeing as they would if they were living elsewhere in the community. This can only be achieved through a whole-system, collaborative approach.
"All parts of the system working together to review the true cause of the presenting issue."
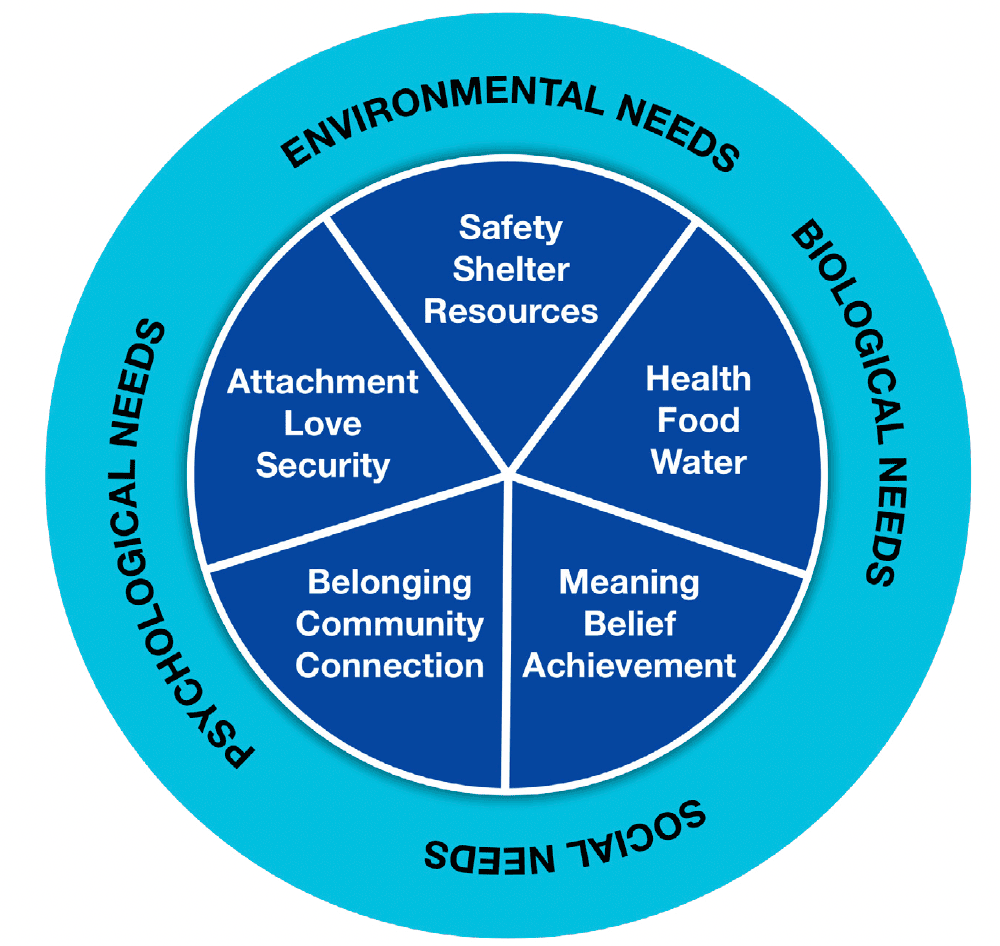
People have a range of health and wellbeing needs that extend across relationships with family and friends. These include psychological and social needs, in addition to environmental needs and basic biological needs. The Wheel of wellbeing diagram (below) helps us to visualise the range of needs, that when fulfilled, contribute to good experiences of wellbeing. All five of the segments within the wheel must be in place to enable optimal health. If one or more of the segments are missing, it can result in a decline in physical or mental health.
The deliberate focus on people, and their health and care, is in recognition of the increasing number and complexity of long term conditions that individuals in a care home are living with. It is also in recognition of the fragmented or reactive healthcare that is often experienced, rather than preventative and planned healthcare.
This new framework specifically seeks to strengthen the continuity and access to healthcare, both from within and outwith the care home. It is about ensuring that people living in care homes have all of their needs met, and are supported to live their best life possible. The first step to achieve this was to have a diverse programme of engagement that encouraged active participation with various stakeholders including those living and working in care homes and their families.
Contact
There is a problem
Thanks for your feedback